Abstract
Introduction: Sarcopenia, defined as low muscle mass and low muscle function and/or reduced physical performance, has been identified as a potential risk factor for adverse outcomes in a variety of conditions like elderly patients and patients with solid tumors. However, fewer studies assessed this association in patients undergoing autologous hematopoietic stem cell transplantation (autoHSCT). With this aim, we performed a retrospective study to evaluate the effect of sarcopenia on complications (such as toxicities, infections and intensive care unit - ICU - admission) and survival after autoHSCT for adults with lymphoma.
Methods: We enrolled 135 patients with lymphoma who underwent autoHSCT between January, 2014 and December, 2017, in a single center. Computed tomography (CT) imaging scans were used for muscle mass analysis. Skeletal muscle area (SMA, cm2) was measured on axial CT images at the level of the third lumbar vertebra (L3) using appropriate software (Slice O´Matic, Tomovision, CA). SMA was normalized for height to obtain the skeletal muscle index (SMI, cm2/m2). We set our own cut-off values at lowest specific tertiles of SMI based on sex and body mass index (BMI, Kg/m2) for diagnosing sarcopenia. Sarcopenia was defined in this cohort as SMI <46 cm²/m² if BMI <25 kg/m² or <51 cm²/m² if BMI ≥25 kg/m² in men, and ≤41.5 cm²/m² in women. Toxicities (overall, renal, hepatic and gastrointestinal) after autoHSCT were graded according to the National Cancer Institute Common Toxicity Criteria (version 4.0). In addition, infections and ICU admission were also analyzed. Patients with previous autoHSCT CT scans more than 120 days were excluded. Probabilities of overall survival (OS), event-free survival (EFS) and treatment-related mortality (TRM) were calculated according to the Kaplan-Meier method. Unadjusted and adjusted analyses were conducted by using Logistic Regression models to determine the association of covariates with outcome. The significance level was adopted at p<0.05.
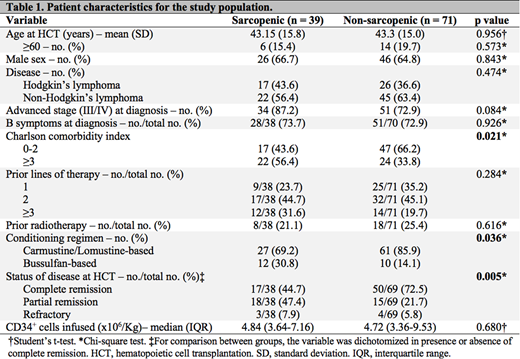
Results: A total of 110 patients met the eligibility criteria (39 sarcopenic and 71 non-sarcopenic). Mean age at transplant was similar in both groups (43 years, p=0.96), with 18% of elderly. The majority of patients was male (65%) and had an aggressive disease at diagnosis (77%). Sarcopenics had a higher Charlson comorbidity index (≥3) at transplant than non-sarcopenics (p=0.02). The conditioning regimen used was different between groups, with a higher proportion of bussulfan-based conditioning in the sarcopenic group (p=0.04). Table 1 list characteristics between sarcopenics and non-sarcopenics patients. Neutrophil recovery was achieved at a median time of 11 days after transplant in both groups (p=0.55). We found association between grade 3-4 gastrointestinal toxicity and sarcopenia (44% vs. 24%; OR 2.46, CI95% 1.07-5.66, p=0.03), although, after adjustment by conditioning regimen, no significant difference was detected (OR 2.09, CI95% 0.89-4.97, p=0.10). No statistically differences were detected in ICU admission, occurrence of infection, hepatic, renal or overall toxicities. Median follow-up of survivors was 20 months (range, 1-50). The 2-years OS and EFS were 72% (CI95% 61-81; sarcopenic 70% [50-84] vs. non-sarcopenic 74% [59-84], p=0.99) and 62% (CI95% 51-71; sarcopenic 68% [49-81] vs. non-sarcopenic 59% [46-70], p=0.37), respectively. The cumulative incidence of TRM was 6.5% at day 100 (CI95% 2.5-11.9; sarcopenic 5.1% [1.3-19.0] vs. non-sarcopenic 5.7% [2.2-14.5], p=0.70).
Conclusion: In our study, sarcopenia was not statistically associated with severe toxicity and higher mortality. To the best of our knowledge, this is the first study to assess CT images and compare sarcopenia with toxicity in aHSCT for lymphoma. Prospective studies are needed to investigate the real impact of sarcopenia on outcomes after autologous transplantation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal